CMS CAHPS Compliance & Reporting: Audit Readiness and Bonus Payments
Atlas Systems Named a Representative Vendor in 2025 Gartner® Market Guide for TPRM Technology Solutions → Read More
Atlas Systems Named a Representative Vendor in 2025 Gartner® Market Guide for TPRM Technology Solutions → Read More
Optimize and secure provider data
Streamline provider-payer interactions
Verify real-time provider data
Verify provider data, ensure compliance
Create accurate, printable directories
Reduce patient wait times efficiently.



4 min read | Last Updated: 20 Jan, 2026
Provider data and health plan directories have been in the news more and more – and the news is often bad. The New York Attorney General reported last year that directories of mental health providers are 86% inaccurate, and a Senate Finance Committee report found that the Medicare Advantage plan was overrun by “ghost networks” – groups of doctors who cannot be contacted or pinned down for appointments.
The problems with provider data accuracy and management often begin with health systems and provider groups, which collect provider information at onboarding and then struggle to keep it current. These organizations play a huge role in the provider data ecosystem, and their effectiveness in keeping that data up to date can affect revenue cycles, new-patient referrals, and even care access.
What are the challenges that health systems and provider groups face in capturing and maintaining accurate provider data? To find out, Atlas Systems recently sat down with two experts in the field:
Let’s hear the challenges they identified, as well as some solutions to consider.
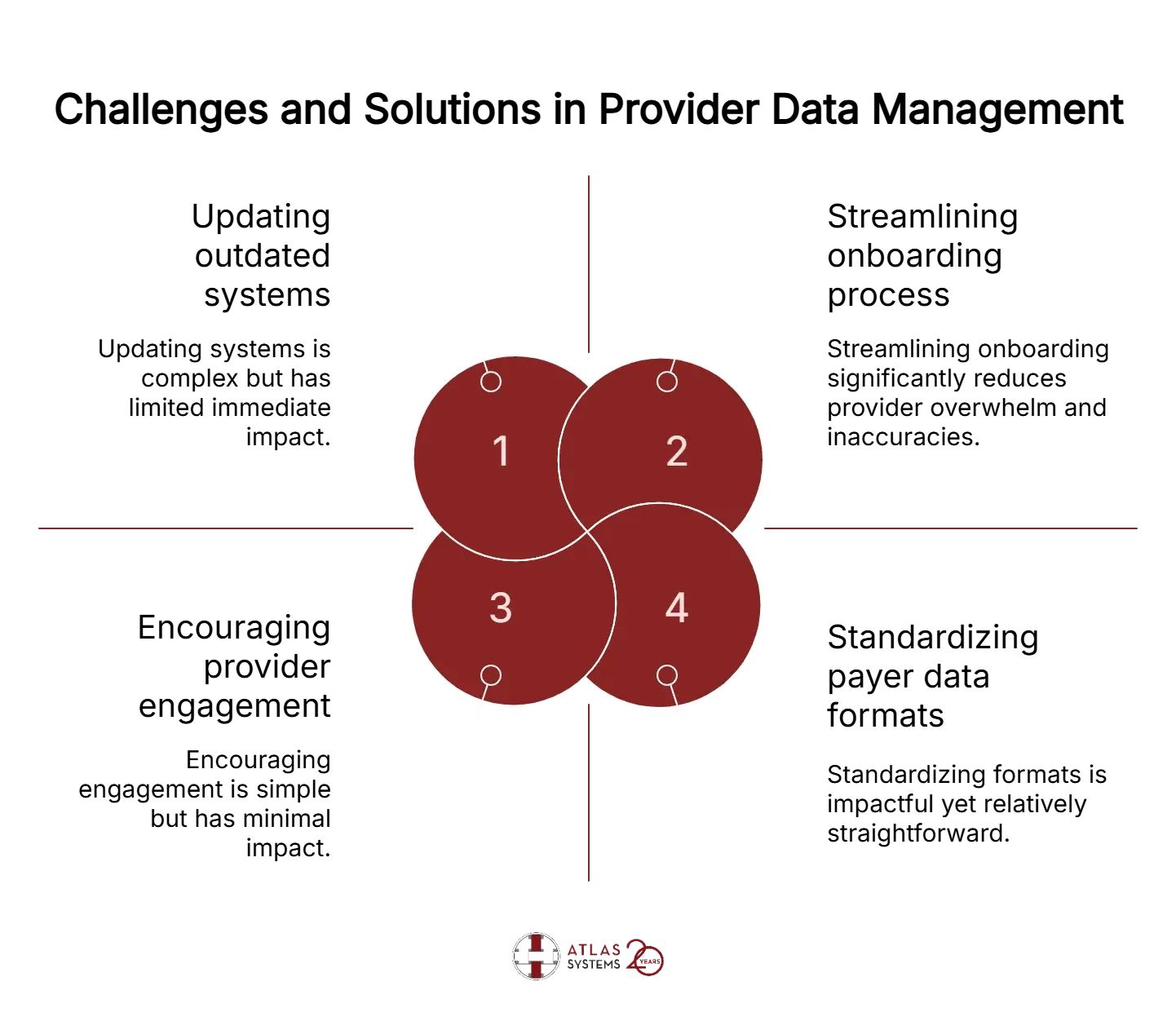
Some of the data challenges that can impact satisfaction of patients and providers alike begin at onboarding. If provider data is not collected and loaded correctly the first time, a lifetime of inaccuracies and confusion may ensue, with bad data snowballing.
“A lot of times the process for onboarding is fractured,” observed Scrivener. ”You've got HR asking [doctors] for information. You have your credentialing team asking them for information. So that provider is being bombarded with requests before they even start working for your entity.
“The first and most important thing to do ,” Scrivener continued, “is to think about creating the most streamlined process you can to help onboard that provider. See if you can find a way to only get one contact to work with the doctor, so that that doctor doesn't feel overwhelmed.”
Setting expectations with providers is also crucial. “The process in the beginning can be tough,” Scrivener explains. “There's a lot of things that we need. So let [providers] know upfront, to make sure you're successful in kicking things off on the right way.”
Working with hiring managers at health systems can also be key, Gillich recalls. “They really want to hire these providers and have them all set, day one, to see patients – but due to data load issues, delays in health plan participation are a huge barrier. We have staff that focus on all of this enrollment, credentialing and demographic data work. They need to carve out a fair amount of time to share information, to set them up correctly at the beginning.”
For the system to keep working well, providers need to keep everybody informed about any changes in their status – address, insurance accepted, specialties, certifications, and more.
“We need to keep them involved,” says Scrivener, “to let us know when changes happen so that we can make sure their profile reflects all of the expertise that they have. Getting them to understand can be challenging sometimes; they're very busy, and they want to take care of the patient – obviously that is the priority. But we need their information to be able to market them correctly and make sure that we can get them reimbursed properly.”
3. Staying ahead of schedule
Because of huge lag times and red tape, remaining on schedule in provider data management often requires staying ahead of deadlines – way ahead. “Being proactive in everything you do is super important,” Scrivener agrees. “At minimum, we ask departments or groups to tell us about a new provider at least 90 days in advance – but we'll even take a provider six months or a year in advance. If you know someone's coming to do a fellowship in a year, let's start now.”
Almost everyone involved in managing provider data reports that the systems and tools are often hugely outdated and clunky. “Some people are still using Excel to track payer enrollment or credentialing information,” Scrivener reports. “Plans are still requiring hard copies of information, which still requires people to have a file on hand that they can pull the information out.”
“Having stepped away from this work for a little bit,” Gillich adds, “I was pretty surprised that the whole process has not changed that much. In my mind, any of those processes that are so manual is most likely healthcare waste in this day and age. Those folks could be spending time doing much more critical, patient-facing work and getting patients access to care.”
Maybe the most common complaint from provider data managers at health systems is that health plans do not coordinate or standardize the data formats they require. “There's no standardization – no healthcare plan has anything consistent with each other,” Scrivener says. “We spend hours preparing submission files to go to plans. It is still a long arduous process.”
“When I was at a payer,” Gillich recalls, “we would make some improvements and think, ‘This is a great improvement.’ And then I would hear back from the practices: ‘Well, you're really 25% of my business.’ When you make these changes, it doesn't really help in the bigger picture, because you're making changes just for your book of business.”
The new PRIME® Provider-Payer Connect from Atlas Systems creates a crucial space for information exchange between health systems and health plans. Atlas is working with providers to apply automation and AI, creating a seamless data transfer in real time, removing all manual work.
“The interoperability is really key,” Gillich explains. “The PRIME system is FHIR standardized. It really gives us that single unified experience that we were talking about between hiring, re-credentialing, and re-certifying and ultimately sharing demographic and other data up and downstream”
Provider-Payer Connect is built to ingest all the multiple different kinds of responses that health systems get from payers and track when it comes back, who fixed it, and how it gets fixed, then send it back to the payers.
Contact Atlas PRIME® at primesales@atlassystems.com
Get a free expert consultation to identify gaps, prioritize high-risk vendors, and modernize your TPRM approach.